November 14, 2025
The Silent Killer: Fighting Ovarian Cancer Through Innovation and Investment
Invest in ovarian cancer innovation with Portfolia’s women-led funds, backing early detection, smarter diagnostics, and treatments that can save more lives.
Topics
Key Takeaways
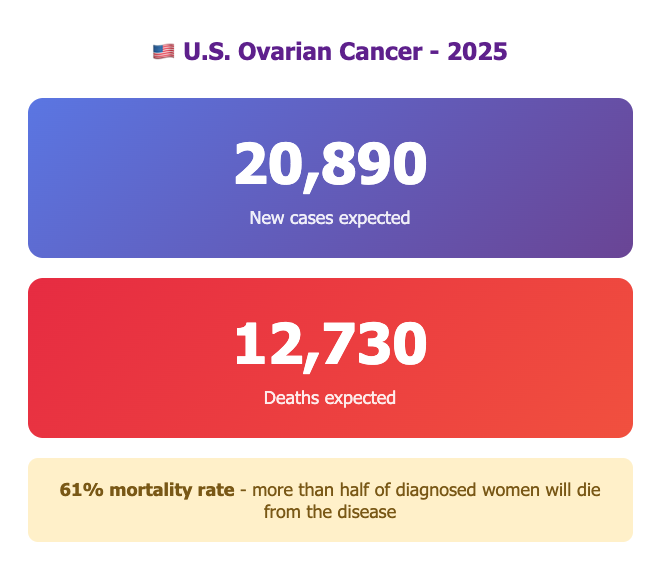
✓ 20,890 U.S. cases, 12,730 deaths expected in 2025
✓ 324,000 global cases, 207,000 deaths annually
✓ 51.6% five-year survival - deadliest gynecologic cancer
✓ 93% survival if caught early vs 20% for advanced stage
✓ NO effective screening test for average-risk women
✓ $70B global economic burden across 11 countries
✓ Rates declining 1.6-2.7% annually - progress being made
✓ Emerging technologies offer hope: AI, liquid biopsy, multiomics
✓ Portfolia leading investment with 46 companies, 100+ investments
Ovarian cancer has earned a grim nickname: the "silent killer." Every year, it claims more lives than any other cancer of the female reproductive system, yet it remains one of the most challenging cancers to detect early. In 2025, an estimated 20,890 women in the United States will be diagnosed with ovarian cancer, and 12,730 will die from the disease—a mortality rate that exceeds both cervical and uterine cancers combined.
Globally, the picture is even more sobering. With over 324,000 new cases and 207,000 deaths annually worldwide, ovarian cancer accounts for $70 billion in socioeconomic losses across just 11 countries. Without better prevention or control measures, projections suggest that ovarian cancer will claim more than 8 million lives between 2022 and 2050.
Yet amidst this crisis, there is hope. Innovation is accelerating, investment is growing, and patient advocacy is intensifying.
Portfolia is one of the leaders in this shift. As the most active investor in women’s health; with a portfolio that includes 46 women’s health companies and more than 100 investments across the sector.Portfolia channels capital from women investors into founders working on diseases like ovarian cancer, where the stakes could not be higher.
This article looks at why ovarian cancer has been so difficult to tackle, where innovation is starting to change the story, and how Portfolia’s investing model supports solutions in this space.
The Scale of the Problem: Why Ovarian Cancer Is So Lethal?
A Small Slice of Cases, a Large Share of Deaths
Ovarian cancer is the 11th most common cancer among women in the United States; but it’s the 5th leading cause of cancer-related death. That imbalance is what makes it so deadly.
At a glance:
- 20,890 new U.S. cases expected in 2025
- 12,730 U.S. deaths expected in 2025
- 324,000 new cases globally each year
- 207,000 global deaths annually
- 1 in 91: A woman’s lifetime risk of developing ovarian cancer
- 1 in 143: A woman’s lifetime risk of dying from ovarian cancer
- 51.6%: Five-year relative survival rate (vs. ~90% for breast cancer)
- ~243,572 women living with ovarian cancer in the U.S. (as of 2022)
- Median age at diagnosis: 63 years
- Median age at death: 70 years
For founders and investors, this is a classic example of an area where need and impact are high, but historical investment has been low. A modest improvement in early detection or treatment outcomes can translate into thousands of lives extended and billions of dollars in value preserved.
Why Ovarian Cancer Is So Hard to Catch Early?
Ovarian cancer is most treatable when found at an early stage. The five-year survival rate for stage I disease is around 93%. The problem is that most people are not diagnosed at stage I.
1. Symptoms That Hide in Plain Sight
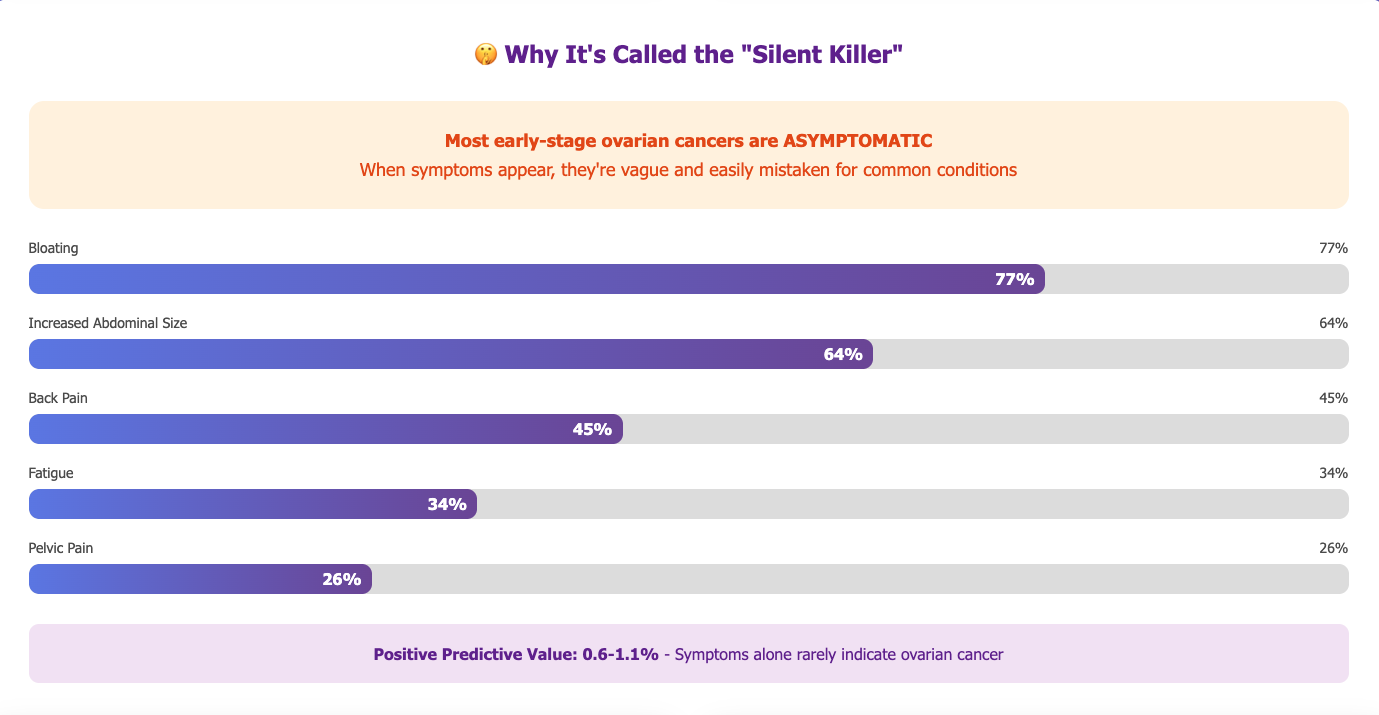
Many early-stage ovarian cancers have no obvious symptoms. When symptoms do appear, they often mimic more common conditions—digestive issues, back pain, or general fatigue—leading to delays in diagnosis.
Commonly reported symptoms include:
- Bloating (reported by ~77% of advanced-stage patients)
- Increased abdominal size (64%)
- Back pain (45%)
- Fatigue (34%)
- Pelvic pain (26%)
- Constipation (24%)
- Abdominal pain (22%)
- Urinary urgency or frequency (16–34%)
On their own, these symptoms have a very low positive predictive value (0.6–1.1%) for ovarian cancer. In other words, they almost never point clearly to the disease which means both patients and clinicians can understandably miss early warning signs.
2. No Effective Screening Test for the General Population
Unlike mammograms for breast cancer or Pap tests for cervical cancer, there is no recommended screening test for ovarian cancer in average-risk women.
Two of the most studied tools have serious limitations:
- CA-125 blood test: Levels can be elevated by benign conditions (such as endometriosis, pelvic inflammatory disease, or even menstruation). At the same time, about half of early-stage ovarian cancer patients do not have elevated CA-125.
- Transvaginal ultrasound (TVUS): It can detect masses but struggles to distinguish benign from malignant lesions, and it has limited sensitivity for early-stage disease. Most masses found on screening are not cancer.
Large studies have shown that using these tools for routine screening in average-risk women leads to more testing and surgeries, without reducing ovarian cancer deaths. As a result, no major medical body currently recommends them for population-wide screening.
3. The “Rarity Problem” in Screening
Even within oncology, ovarian cancer is relatively rare. Its annual incidence in the general population is roughly 0.09%. That creates a math problem: even a test with 90% sensitivity and 90% specificity would still have a positive predictive value of only about 1%. That means 99 out of 100 positive tests would be false positives, leading to unnecessary anxiety, invasive procedures, and cost.
From a product and innovation standpoint, this is the central technical challenge: how do we build tools that catch early disease without overwhelming patients and healthcare systems with false alarms?
The Economic Toll: Personal, Systemic, and Global
Ovarian cancer’s impact goes far beyond clinical outcomes. It has a heavy economic and social cost for patients, caregivers, health systems, and economies.
Patient-Level Financial Burden
- ~$100,000: Average cost of care in the first year after diagnosis
- ~$3,000: Average patient out-of-pocket spending in that first year (about 3% of total costs)
- $200,000+: Total economic burden can exceed this amount annually depending on stage and treatment
- 4x higher: Median medical cost for ovarian cancer vs. uterine or cervical cancer
- 22 additional workdays missed per year compared to non-cancer patients
Health System and Workforce Impact
- $3.8 billion: Annual U.S. medical expenditure for gynecologic cancers (ovarian cancer is second costliest overall, but highest per patient)
- 2.5 million workdays lost due to illness
- 9,403 women effectively “missing” from the workforce (survivors unable to return)
- 3,663 years spent by patients traveling to or receiving treatment
- 17,112 person-years of caregiver time (average 33 days per patient)
Inequity and Income Disparities
In the first two years after diagnosis, treatment costs equate to:
- 7× total health spending per capita in high-income countries
- 41× in upper-middle-income countries
- 118× in low- and lower-middle-income countries
For innovators, this underscores a dual mandate: better clinical outcomes and better financial outcomes. Solutions that detect earlier, reduce treatment intensity, shorten hospital stays, or streamline care have the potential to dramatically lower both human and economic costs.
Emerging Technologies: Where Innovation Is Changing the Story?
Despite decades of slow progress in screening, the landscape is now shifting. Multiple technology waves are converging on ovarian cancer.
New Frontiers in Detection and Monitoring
1. Liquid Biopsy
Blood-based tests that look for circulating tumor DNA (ctDNA) or microRNAs are advancing quickly. Although early-stage detection remains challenging, liquid biopsies are showing promise for both diagnosis and treatment monitoring.
2. Multiomics Integration
Combining genomics, proteomics, metabolomics, and other “omics” layers can reveal more precise biomarker signatures. These multi-dimensional profiles may eventually enable better risk stratification and earlier detection.
3. Artificial Intelligence and Machine Learning
AI is being used to improve imaging interpretation, recognize subtle patterns in ultrasound or CT scans, and analyze complex biomarker data. Smarter algorithms can potentially increase sensitivity and specificity without overwhelming clinicians with false positives.
4. Advanced Imaging Techniques
New modalities including photoacoustic imaging, functional imaging, and advanced PET/CT—offer more detailed views of tumors, microvasculature, and metabolic activity, which could support earlier and more accurate diagnosis.
5. Multipanel Biomarker Tests
Moving beyond single markers like CA-125 to panels of proteins and other biomolecules is one of the most promising directions. In one study, monitoring dysregulation of four protein markers identified women one to two years before clinical diagnosis with an AUC of 0.848.
6. Genetic Risk Stratification
Identifying women with BRCA1/2 mutations and other high-risk variants allows for more intensive surveillance and preventive options (such as risk-reducing surgery), shifting focus from late-stage treatment to risk management.
These technologies don’t just represent scientific progress—they form the foundation of new diagnostic companies, digital platforms, and care models that investors can support.
Signs of Progress: Declining Incidence and Mortality
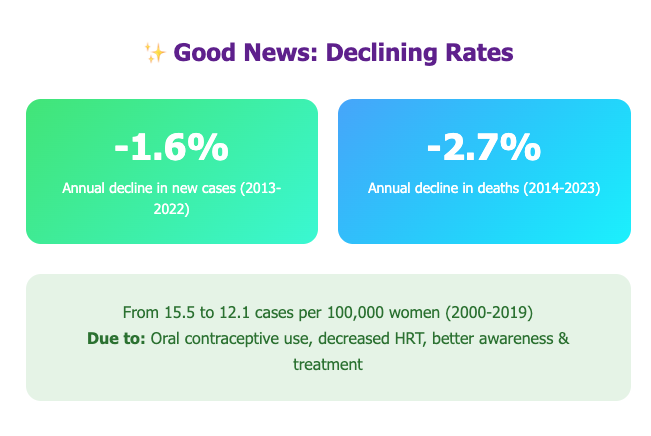
Amid the urgency, there are real signs that collective efforts are making a difference:
- New ovarian cancer cases have been declining by about 1.6% per year on average (2013–2022)
- Death rates have declined by roughly 2.7% per year on average (2014–2023)
- Age-adjusted incidence in the U.S. dropped from 15.5 to 12.1 cases per 100,000 women between 2000 and 2019
- From 2015 to 2019, incidence fell more steeply—from 13.4 to 12.1 cases per 100,000 (a 2.4% annual decline)
These trends are linked to factors such as greater use of oral contraceptives, reduced use of certain menopausal hormone therapies, increased awareness, and advances in treatment.
But even with these improvements, ovarian cancer remains one of the most lethal cancers affecting women. There is still a wide gap between the outcomes we have and the outcomes we want.
How does Portfolia invest in Ovarian Cancer Innovation?
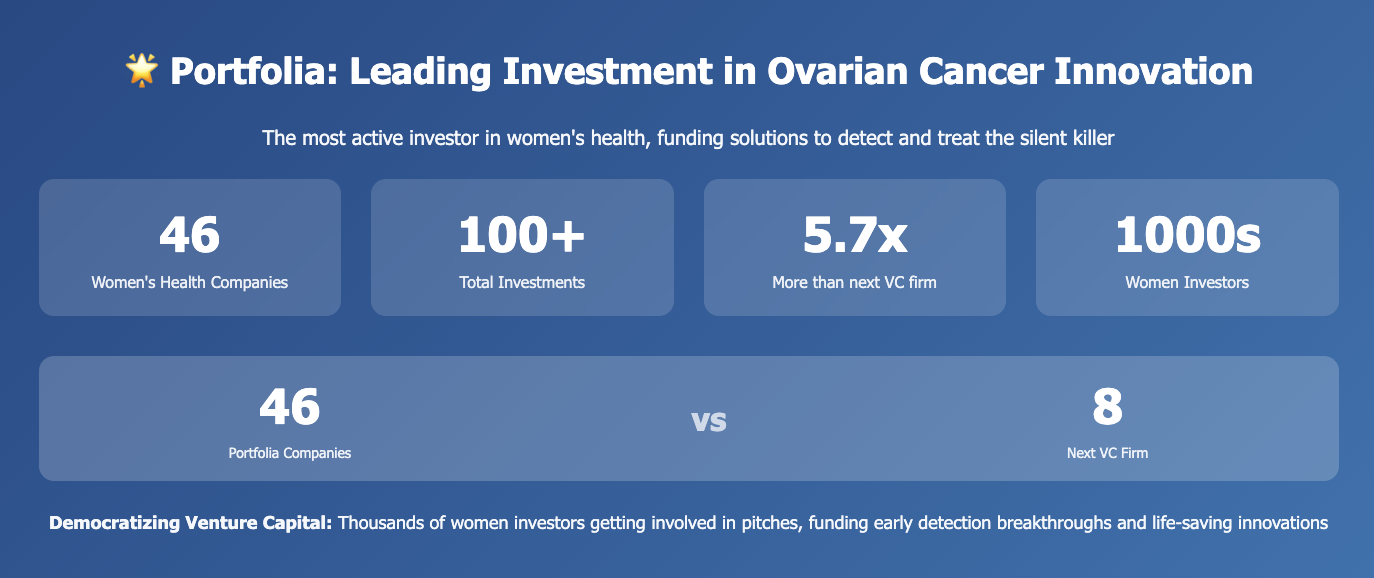
Historically, women’s health and gynecologic cancers in particular have been underrepresented in venture portfolios. Many funds shy away from complex oncology categories with longer timelines and specialized science.
Portfolia was built to do the opposite: to intentionally move capital into areas where women’s health needs are urgent, outcomes lag behind, and traditional investment is light.
Within women’s health, ovarian cancer fits that profile:
- High mortality relative to incidence
- Major quality-of-life and economic burden
- Clear scientific questions and technological opportunities in early detection and treatment
Portfolia’s women’s health funds:
- Focus on founders tackling hard problems like ovarian cancer, not just incremental improvements in better-known categories.
- Draw on a community of thousands of women investors, many of whom have personal or family experience with cancer.
- Bring together expertise from oncology, diagnostics, data science, payer and provider systems, and patient advocacy.
Rather than just writing a check, Portfolia’s model creates a feedback loop between founders and investors: investors bring lived experience and domain knowledge; founders bring cutting-edge science and technology; together they refine solutions that are both clinically meaningful and commercially viable.
Portfolio Spotlight: Innovators Targeting Ovarian Cancer
Within Portfolia’s broader women’s health ecosystem, several companies are directly or indirectly changing the outlook for ovarian cancer. Two examples illustrate the range of approaches:
1. Mercy Bio – Making Early Cancer Detection As Simple As a Blood Test
What they’re building
Mercy Bio is developing blood-based diagnostics aimed at catching cancer—including ovarian cancer—at its earliest and most treatable stages.
Why it matters for ovarian cancer
Because ovarian cancer rarely presents with clear early symptoms and lacks an effective screening test, many diagnoses occur only after the disease has spread. Mercy Bio’s platform analyzes genomic and proteomic biomarkers from a standard blood draw to identify cancer signatures far earlier than current methods.
The potential impact
If clinicians can reliably flag high-risk patients before tumors become advanced, survival rates could increase, treatment regimens could be less aggressive, and overall costs could be significantly reduced. Making early detection as straightforward as a blood test is a powerful step toward transforming ovarian cancer from “silent killer” to “detectable disease.”
2. FemDx Medsystems – Bringing Better Cancer Diagnostics Into the Exam Room
What they’re building
FemDx Medsystems is designing minimally invasive diagnostic devices that help clinicians evaluate gynecologic tissues more accurately in an office setting.
Why it matters for ovarian and related cancers
Ovarian cancer often sits at the end of a diagnostic chain that begins with nonspecific gynecologic symptoms. By improving how OB/GYNs assess abnormal findings and triage patients, FemDx can shorten the diagnostic journey and reduce missed or delayed cancers—both ovarian and related gynecologic malignancies.
The potential impact
More precise, real-time assessment at the point of care means fewer unnecessary procedures for low-risk patients and faster escalation of care for those who need it most. That can improve outcomes, reduce anxiety and costs, and make better use of specialist and oncology resources.
From “Silent Killer” to Detectable, Treatable Disease: The Path Forward
Ovarian cancer has worn the “silent killer” label for far too long. A five-year survival rate of just over 50%, global economic losses of $70 billion across a small set of countries, and projections of 8 million deaths by 2050 underscore the urgency.
Changing that story will require progress on multiple fronts:
1. Accelerating Early Detection Research
Continued investment in liquid biopsy, biomarker panels, multiomics, and AI-driven imaging to enable detection at earlier stages when survival rates are dramatically higher.
2. Expanding Access to Genetic Risk Assessment
Making BRCA and other risk testing more widely available so high-risk women can access enhanced surveillance, risk-reducing strategies, and targeted therapies.
3. Advancing Treatment Options
Supporting innovation in targeted therapies, immunotherapies, and personalized medicine that improve survival while managing side effects and cost.
4. Addressing Cost and Access Barriers
Developing models that reduce the financial toxicity of treatment, especially in low- and middle-income settings where costs can be over 100 times per capita health spending.
5. Strengthening Awareness and Navigation
Educating women and clinicians about symptoms and risk factors, and improving navigation through complex diagnostic and treatment pathways.
Portfolia’s role in this future is to ensure that capital, expertise, and lived experience converge in the companies working on these problems. With 46 women’s health companies and over 100 investments already in place, Portfolia is helping build an environment where ovarian cancer innovation can move from the lab into clinics and lives.
Help Change the Ovarian Cancer Story
Ovarian cancer will not be transformed by science alone. It will be transformed when breakthroughs are matched with the right kind of capital and a community determined to bring them to patients.
If you believe that early detection, smarter diagnostics, and better treatments for ovarian cancer should move faster, we invite you to explore how Portfolia invests in this space and where ovarian cancer fits within our women’s health funds. Contact our team to get started.
Add your voice, your expertise, and your capital to a community that is backing founders on the front lines of this disease. Together, we can help move ovarian cancer from a “silent killer” toward a future where it is detected earlier, treated more effectively, and, ultimately, far less deadly.
Sources and References
- National Cancer Institute SEER Program. (2025). Cancer Stat Facts: Ovarian Cancer.
- American Cancer Society. (2025). Key Statistics for Ovarian Cancer.
- Ovarian Cancer Research Alliance (OCRA). Ovarian Cancer Statistics & Survival Rates.
- World Ovarian Cancer Coalition. (2024). Ovarian Cancer Data Briefing.
- World Cancer Research Fund. (2025). Ovarian Cancer Statistics.
- Diagnostics. (2025). Early Diagnosis of Ovarian Cancer: A Comprehensive Review.
- Gynecologic Oncology. (2024). Ovarian cancer think tank: Current status of screening.
- Journal of Clinical Oncology Global Oncology. (2024). Socioeconomic Burden of Ovarian Cancer in 11 Countries.
- The American Journal of Obstetrics & Gynecology. (2024). Economic burden